Behind the Stethoscope: Dr. Jay
Behind the Stethoscope is a series where I interview doctors to learn more about their journey, specialty, and passions. A new interview with a different doctor is released with each edition of the Keynote.
Performing surgery is a serious responsibility. The patient on the operating table is trusting the surgeon to physically change them using tools like scalpels, trocars, staples, and sutures, and the procedure can carry significant, and even life-threatening, risks. You expect a surgeon’s personality to match the gravity of the matter. But my uncle, Dr. Nirmal Jayaseelan, isn’t your typical surgeon. He always cracks a joke that gets everyone laughing. When I shadowed him, I saw how he used his humor and caring personality to forge strong connections with patients and make them feel comfortable even though they are in a scary position. This care extends to his healthcare team, who greeted him with excitement when we arrived at the surgical center because they were so happy to work with him (plus, he brings donuts every time, and we all know the way to one’s heart is through a donut).
Having performed more than 8,000 weight-loss surgeries, Dr. Jay is one of the most experienced bariatric surgeons in the nation. In this interview, he talks about what he does as a bariatric surgeon, the gastric sleeve procedure, the stigma for people considering bariatric surgery, the oddly relaxed atmosphere in the operating room, and more!
What types of patients do you see, and how does bariatric surgery affect their lives?
I see a wide variety of patients from 12 year olds to age 70. Some have only 50 pounds to lose, and some have 500 pounds or more to lose. Bariatric surgery can cure Type 2 diabetes; improve heart, lung, liver and kidney function; treat back, hip, knee and foot pain by reducing stress on joints; and reduce depression and anxiety.
What is bariatric surgery?
Bariatric surgery operations are performed on the stomach or intestines to help patients who are 50 or more pounds overweight lose weight. However, specializing in bariatric surgery means we treat all facets of the patient with a team of people. There are nutritionists, psychologists, and personal trainers.
Being 50 or more pounds overweight is a metabolic trap. Studies have shown only 5% of people who start a diet and exercise program after five years will maintain or lose weight; 95% gain weight.
Surgery, close follow up, and new medications can reverse this trend. Currently, the most popular weight loss surgery is the gastric sleeve. It is a laparoscopic surgery which means it’s done through tiny holes the size of a pencil. You can take your shirt off to swim, and no one can tell that you had surgery. It’s about a thirty-minute surgery. Most people have the surgery on Thursday and go back to work on Monday.
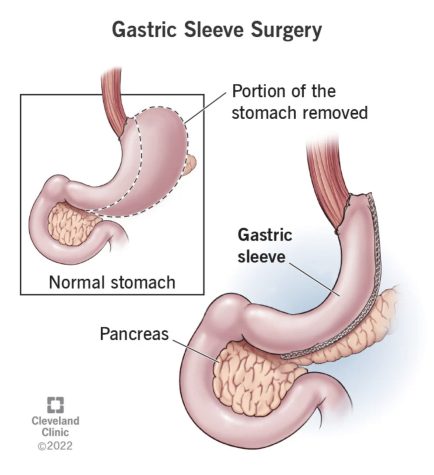
Your stomach is a balloon about the size of your hand that can stretch out and hold about two plates of Thanksgiving dinner. When we do a gastric sleeve, we cut the stomach to the size of a large banana, about half the size of your hand. It takes about three weeks for the sutures on the stomach to heal, so for three weeks, the patient needs to be on a liquid diet like protein drinks, smoothies, or soups. If patients accidentally eat in the first three weeks, solid food can break a suture, and the stomach can leak, leading to bad infections in the abdomen and prolonged hospitalization.
How do you follow-up with patients after their surgery?
Postoperatively, I like to see patients weekly to ensure they are sticking to the liquid diet. After three weeks, patients slowly advance to a regular diet. A standard meal my patients will eat is a small chicken breast and a small salad, but they will feel like they ate Thanksgiving dinner due to the surgery.
Long-term bariatric surgery does a good thing, which is helping patients burn up fat, but it does a bad thing by also burning up muscle. Patients must eat adequate protein and lift light weights to prevent muscle loss. Also, with a smaller stomach, absorption of vitamins and minerals is diminished, so eating lots of green, colorful vegetables and fruits is vital. We routinely check the patient’s blood every six months after surgery to make sure all the vitamin levels are normal and they’re not anemic.
Why were you drawn to bariatric surgery?
As a medical student, my rotation in surgery was so much fun. The residents were so nice to me, and they seemed very satisfied with choosing surgery. Now as a surgeon, I feel very happy with my choice. It is hard work to get here, but any kind of success requires hard work to attain. Bariatric surgery makes a dramatic improvement in people’s health as well as self esteem. It’s a happy specialty like delivering babies.
Is weight mostly impacted by lifestyle choices like diet and exercise, or is a large part also genetic and out of a patient’s control?
Weight gain is multifaceted. Yes, genetics and lifestyle are important, but also metabolic changes during puberty, pregnancy and menopause affect weight gain. But once fat cells are formed, they do everything in their power to survive, and we are just starting to learn the metabolic power of adipose tissue.
I think a lot of people would initially feel that bariatric surgery is a cosmetic surgery catering to beauty standards rather than improving health outcomes. What would you say to those people?
Losing five pounds with liposuction is cosmetic. Losing weight to treat your health is not cosmetic surgery.
Is there a stigma for patients who want bariatric surgery? Are patients often insecure about their weight? Do you think other health professionals may be contributing to this insecurity?
Yes, yes, and yes. Obese patients are looked down upon. They are definitely mistreated in our society. People say go on a diet or workout, but my patients have been working out and dieting for years. In the last 20 years, other healthcare professionals have begun referring patients to bariatric surgeons for help, especially orthopedic surgeons who want patients to lose weight before fixing their back or replacing a hip or knee joint.
When I had the privilege of shadowing you, your personal investment and care for your patients and the people you work with was immediately clear. How do you think your positive, humorous, caring personality affects your patient care?
As a physician you have to be able to communicate effectively with patients. Being able to read the room and inject some humor appropriately is a plus. Also, people can tell if you actually care about them or if you’re just going through the motions.
When I think about an operating room, I imagine a tense and serious atmosphere, probably based on portrayals on TV. But when I watched you in the operating room, I was surprised by the calm atmosphere with music and normal conversation and banter. Why is the atmosphere in the operating room this way?
The operating room is like being on a soccer team. Everyone has a certain role. Music, conversation/banter and humor keep my team relaxed and engaged in the operation. Tension and struggling should be avoided in surgery. As a resident, I learned that surgeons that were tense and stressed often struggled and had poor outcomes.
Where do you foresee the future of weight loss medicine going? Do you think that it is feasible that within a few decades the invasive procedures you are performing could be replaced with noninvasive approaches?
In the short term, new injectable weight loss meds are helping immensely. Patients can lose 20 pounds with very few side effects. Endoscopic (through the mouth) procedures for weight loss have been around for 15 years but have not become reliable yet. Robotic surgery is currently a mainstay in bariatric surgery, and it will be ubiquitous in all surgery in the next 20 years.
Thank you, Dr. Jay!
I hope you enjoyed learning about Dr. Jay and the field of bariatrics. The next edition of Behind the Stethoscope comes in February. Until then, happy holidays!

Niraj is a current Senior at Keystone who is interested in spreading awareness about health issues and inequality through his writing. He is fascinated...

